Table of Contents
pre-excitation syndromes including WPW
see also:
introduction
- pre-excitation occurs when some portion of the ventricles are activated by an impulse from the atria sooner than expected if passing down a normal pathway.
- various forms have been described and are believed to be due to accessory tracts that bypass all or part of the conducting system:
- James fibers are a continuation of the posterior internodal tract and connect the atrium and proximal His bundle
- atrial impulses can therefore completely bypass the AV node to activate the ventricles resulting in:
- short PR interval as the AV node is bypassed
- normal QRS because the fibers insert directly into the infranodal conducting system
- when this is associated with re-entrant SVT, the clinical condition is termed Long-Ganong-Levine syndrome (LGL)
- the short PR interval in LGL is typically caused by accelerated conduction through the atrioventricular (AV) node, rather than an accessory pathway as seen in Wolff-Parkinson-White syndrome. However, in some cases, the short PR interval may be due to the presence of an accessory pathway composed of James fibers.
- Mahaim bundles are composed of myogenic tissue from either AV node, His bundle, or bundle branches and insert into the ventricles in the septal region
- atrial pulses thus pass through the AV node but ventricular activation is via two sources - the Mahaim bundle and the normal pathway, hence:
- normal PR interval
- initial distortion of the QRS (delta wave)
- Kent bundles are composed of myogenic tissue and directly like the atria to the ventricles, completely bypassing the AV node and infranodal system, thus:
- if anterograde conduction:
- short PR interval
- initial distortion of the QRS (delta wave)
- if no anterograde conduction is possible (as in 20% with WPW), normal QRS and no delta wave but can sustain a orthodromic re-entrant SVT.
- there are various types of Wolff-Parkinson-White syndrome (WPW):
- type A:
- ventricular activation first occurs in inf-post portion of LV ⇒ delta wave directed anteriorly ⇒ +ve deflection with dominant R in V1 with inf Q waves.
- type B:
- ventricular activation first occurs in inf-post portion of RV ⇒ delta wave directed posteriorly and left ⇒ -ve deflection and rS or QS in V1
- type C:
- ventricular activation first occurs in post-lat portion of LV ⇒ delta wave directed right, superiorly & anteriorly ⇒ +ve deflection V1 with negative or iso-electric delta wave in V5-6.
- because there is altered depolarisation, repolarisation is often abnormal with resultant ST - T changes which may mimic infarction or ischaemia
- type A may mimic posterior MI
- type B may mimic inferior MI
Wolff-Parkinson-White syndrome (WPW)
clinical features:
- high incidence of tachyarrhythmias - atrial flutter in 5%, AF in 10-20%, and paroxysmal re-entrant SVT in 40-80%
- re-entrant SVT occurs when an impulse is sustained in a loop composed of the bypass tract and the AV conducting system
- whether the QRS is normal or wide dependws on whether the anterograde direction is through the AV conducting system (orthodromic - occurs in 80-90% of cases and there is no delta wave present and there is a normal QRS) or via the accessory pathway (antidromic ⇒ wide QRS and a delta wave may be visible).
- rentry is usually initiated by a premature atrial contraction which encounters a bypass tract which is still refractory from the previous sinus beat, but the AV node has recovered partially and conducts the impulse more slowly than normal.
- patients with WPW and AF or atrial flutter:
- most patients with WPW, the refractory period in the accessory pathway is longer than in the AV node
- some patients with WPW, the refractory period in the accessory pathway is shorter than in the AV node so more atrial impulses can be conducted through to the ventricles via the accessory pathway resulting in wide QRS complexes and potential for atrial flutter with 1:1 conduction and life threatening ventricular rates of 300/minute. This can also occur in AF, particularly if anti-arrhythmics are used which block the AV node such as beta blockers and calcium channel blockers.
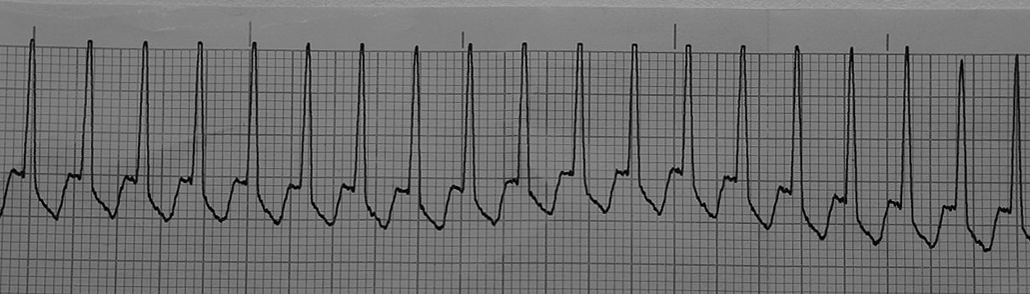
ECG of patient with WPW post DC reversion from antidromic AVRT:
Mx of SVT due to WPW
orthodromic, narrow QRS re-entrant SVT
- can be treated as for other causes of narrow complex tachycardias such as with:
- vagal maneuvers as 1st line
- adenosine or verapamil (Isoptin) as 2nd line if no C/I
- if above fail, then procainamide
- 20 to 50 mg/minute given intravenously while monitoring the blood pressure closely every 5 to 10 minutes until either:
- the arrhythmia terminates
- hypotension ensues
- the QRS is prolonged by more than 50 percent, or,
- a total of 17 mg/kg [1.2 g for a 70 kg patient] has been given
- some patients may convert to broad complex antidromic AVRT following Rx with adenosine
- if unstable, then DC cardioversion
- beta blockers are usually ineffective
permanent junctional reciprocating tachycardia
- a rare, persistent tachycardia with a long RP interval mainly occuring in children and is generally refractory to medical Mx and requires ablation to cure
- flecainide may be useful whilst awaiting ablation
antidromic, broad complex re-entrant SVT
ambulance rhythm strip after iv adenosine 6mg to Rx the orthodromic SVT shown above:
- usually associated with a short refractory period accessory pathway and thus at risk of rapid ventricular rates and resultant VF
- avoid adenosine, beta blockers and calcium channel blockers in cases of broad complex tachyarrythmias with WPW unless it is definetely antidromic AVRT and not AF or atrial flutter otherwise there is a risk of VF
- if unstable, then DC cardioversion
- if stable, then consider iv procainamide
Mx of atrial flutter or AF in WPW patients
- AV nodal blockers may cause VF, particularly verapamil!
- adenosine, beta blockers and calcium channel blockers should all be avoided
- digoxin is also C/I as it may shorten the refractory period and cause rapid ventricular rate and VF
- sync DC cardioversion may be the best choice if cardioversion is required or the patient is unstable
- be ready to Rx VF with unsynchronised defibrillation as DC reversion risks inducing VF if the defibrillator misidentifies T waves as R waves and delivers a R on T shock1).
- reduce this risk by:
- select a lead which maximises R wave height
- select a higher energy initial shock (120-200J) as this is less likely to induce VF than low energy shocks
- manually check synchronisation accuracy by printing a rthythm strip and review the sync arrows
- time the shock to be in a longer R-R interval
- alternatively, consider using drugs which prolong the refractory period of the accessory pathway such as procainamide or flecainide.
- see also AF
1)
Taylor. EMA (2013) 25, 612-613