hypoxia
Table of Contents
hypoxia
see also:
oxygen content in blood in mls/L = (Hb in g/L x 1.36 x oxygen saturation/100) + (0.03 x PaO2 in mmHg)
introduction
- hypoxic hypoxia can be arbitrarily defined as arterial oxygen partial pressure of less than 80mmHg in room air
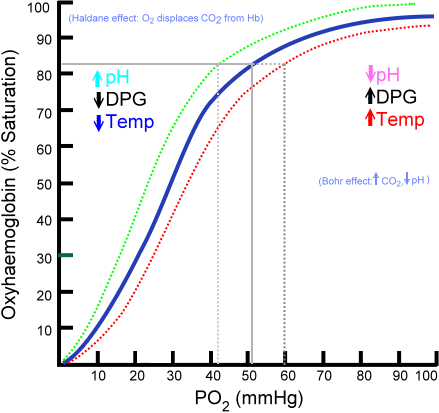
- an arterial PO2 < 60mmHg indicates respiratory failure as, at oxygen levels below this, the Hb-oxygen dissociation curve is steep which means that the ability for Hb to carry much oxygen to the tissues is markedly diminished, as it evolved to be off-loading oxygen to the tissues at these pressures.
- pO2 of 60mmHg equates to an oxygen saturation of less than 90% (see Hb-oxygen dissociation curve - see wikipedia)
- other causes of “hypoxia” or insufficient cellular oxygen usage include:
- anaemic hypoxia - insufficient haemoglobin to carry the oxygen in the blood
- impaired oxygen delivery due to carbon monoxide poisoning or methaemoglobinaemia
- ischaemic hypoxia due to impaired blood flow such as from either blockages, vasoconstriction or venous stagnation
- histotoxic hypoxia due to impaired cellular utilisation of oxygen such as with cyanide poisoning
- the following assumes we are discussing hypoxic hypoxia
alveolar gas equation
- an understanding of this equation if critical in emergency medicine
- each minute, a human at rest consumes ~4ml oxygen per kg body weight and produces ~3ml carbon dioxide per kg body weight
- the ratio of CO2 produced to oxygen used is the “respiratory quotient”
- normal alveolar ventilation = 5L/min in adults with a tidal volume approx. 500ml (7ml/kg)
- FiO2 = fraction of oxygen in inspired gas
- for room air, this is 0.21, for 100% oxygen, this is 1.00
- Patm = atmospheric pressure = 760mmHg at sea level (approx) = 101kPa = 12.8 psi
- Pwater = saturated water vapour pressure at body temperature and at prevailing atmospheric pressure = 47mmHg
- PaCO2 = arterial carbon dioxide partial pressure in mmHg (normal ventilation = 40mmHg)
- RQ = respiratory quotient = 0.8 for most people
- if FiO2 is low, the equation can be simplified by approximating FiO2 x (1-RQ) = 0
alveolar PO2 = FiO2 x (Patm - Pwater) - (PaCO2 x (1-FiO2[1-RQ]))/RQ
Alveolar-arterial gradient
- another essential concept to understand in emergency medicine
- an increased A-a gradient suggests their is a pulmonary oxygen transfer aetiology to hypoxia such as impaired diffusion, V/Q mismatch, or right-to-left shunt
- normal range is 5-20mmHg, increasing by 1mmHg for every decade in age
A-a gradient = alveolar PO2 as determined from the alveolar gas equation - actual measured arterial PaO2
causes of hypoxic hypoxia
low inspired oxygen levels
- high altitude
- enclosed spaces
hypoventilation
- in this case there is a rise in arterial PCO2 levels
- obstructed airway
- decreased conscious state - eg. stroke (CVA), toxicology
- exhaustion from work of breathing
- painful breathing - shingles, pleurisy, fractured ribs, etc
- muscle paralysis - toxinology, neuro-muscular blockers, neuropathies
- chest wall pathology or injury
impaired pulmonary oxygen transfer
- pulmonary fibrosis
- congenital heart disease with right to left shunt
- other pulmonary pathology
Rx of hypoxic hypoxia
- ensure adequate airway and ventilation
- may require positive pressure ventilation such as BiPAP or via intubation
- increase FiO2 as needed
- improve lung function
- Rx the cause where possible
- in suitable patients, when severe hypoxic hypoxia persists despite the above:
- consider ECMO
- in the future, whilst awaiting ECMO, we may be able to give an immediate iv infusion of John Kheir's idea of oxygen filled nanoparticles which seem to work in preliminary testing
hypoxia.txt · Last modified: 2014/07/29 07:24 by 127.0.0.1